
Lichen sclerosus disease is a skin disorder, which is most commonly seen in the genital area of women. What is lichen sclerosus? In whom does it occur? What kind of complaints does it cause? What are the symptoms? How is lichen treated?
Lichen sclerosus disease is a skin disorder of unknown cause, which thins the skin, sometimes causes wounds, and may become cancerous when untreated. It is 6 times more common in women than men. It can involve any part of the skin in the body but mostly involves the genital area. If the disease is in the genital area, it is called “Vulvar Lichen Sclerosis” (VLS) or “Genital Lichen Sclerosis”.
“Lichen sclerosus” is a chronic, progressive skin disorder that causes atrophy (thinning),scar tissue and permanent deformity in the skin. It is not a too common disease in the society, but can have serious consequences when not treated in time. It has no definitive treatment, and the treatments available are intended to stop the progression of the disease and reduce the complaints.
Lichen sclerosus is a chronic disease, initially characterized by ivory papules and plaques with definitive borders in the skin and mucosa and then by the development of atrophy (thinning of the tissue). Lichen sclerosus is also known by other medical names such as ‘Lichen disease’, ‘Lichen sclerosus et atrophicus’, ‘Kraurosis vulvae’.
Lichen sclerosus disease most often cause complains of itching in the genital area. In addition, burning sensation, stinging, pricking in the genital area and irritation due to friction while wearing pants, are some other commonly observed complaints. On the other hand, it may cause complaints such as inability to urinate or difficulty in urinating (dysuria) if it involves the front of the urethral orifice, and may cause inability to menstruate if it involves the menstrual canal. It can also cause sexual problems to a considerable extent.
The sexual problems caused by lichen disease include:
Marital problems can also be experienced due to such sexual problems.
Lichen sclerosus is classified into two groups as genital and extra-genital (areas other than the genital area) in terms of the region it involves. It can develop in any part of the skin, but most often involves the genital area. In cases of extra-genital involvement, the disease most commonly develops in the neck, hips, inner thighs, shoulders and wrists.
“Vulva” refers to the external female genitalia, and lichen sclerosus in this area is called "Vulvar Lichen Sclerosus" (VLS). Its spread is highly variable. As the classical literature information, it involves the vulva, perineum and anus area in a “figure of 8” configuration. However, it can also involve just a single region, for example the area around the anus, clitoris, labia minora, labia majora or vaginal introitus.
In almost all cases, the vulva shrinks and changes shape over time. Sometimes the clitoris can be completely buried by fusion. Vaginal entrance can be permanently narrowed as well. However, lichen formation in the vaginal canal is very rare.
Genital Lichen sclerosus is common especially in 50s, and after the menopausal period. However, it can affect all age groups from childhood. One-third of all cases occur under the age of 50. In the pediatric group, lichen sclerosus develops in the first few years of life and involves the genital are in almost all cases.
When untreated, lichen sclerosus can leave permanent, considerable scars. In cases of life-long untreated lichen sclerosus, the risk of transformation into malignant squamous cell carcinoma (cancerous) was found to be 2-6%. Lichen sclerosus is difficult to manage, but it is a disease that can be controlled with treatments at early stages.
Due to poor diagnosis and low level of awareness, its exact incidence rate in the community is unknown. In dermatology outpatient clinics, 10% of newly diagnosed cases related to genital area are found to involve vulvar lichen sclerosus. Another study reported that the ratio of patients diagnosed with vulvar lichen sclerosus during general gynecological examinations was around 1.7%. According to a study conducted in the Netherlands, the incidence rate of lichen sclerosus was 14.6 per 100,000 woman-years. In another study, one of every 59 women was found to have lichen sclerosus.
Vulvar Lichen sclerosus (VLS) usually shows symptoms in women who are in their middle and late 50s. Itching is the most common symptom in adults, and exists in 93% of patients. Itching is more intensive at nights and causes sleep problems. Complaints also include skin abrasions, cracks, dryness and related pain.
In cases of extensive genital involvement, painful sexual intercourse (dyspareunia) or inability to have sexual intercourse can be encountered. Some cases may also involve clitoral hyperesthesia, i.e. extreme sensitivity of the clitoris. Painful urination (dysuria),bleeding from skin cracks and sexual dysfunction are some of the other complaints.
Sometimes women who have no complaints can be diagnosed with this disease during a routine gynecological examination. Its progression without showing symptoms may be more risky in terms of its transformation into cancer. Therefore, yearly gynecological examinations are of great importance.
The etiology of Vulvar Lichen Sclerosis, i.e. the cause of this disease is not clearly known. There are four main causes, which are studied mostly:
1. Autoimmunity, Molecular Mechanisms and Genetic Factors
Although auto antibody levels are found to be high in studies on autoimmunity, it cannot be said that this is the exact cause. 30 percent of patients have a family story. Autoimmune thyroiditis (Hashimoto) and vitiligo are the two most common diseases accompanying it. It is also thought to be associated with morpheo, alopecia areata, and pernicious anemia. Studies have reported cases accompanied by diabetes mellitus, psoriasis and celiac disease. However, their coexistence could be coincidental. A high incidence like 17% was found in patients with Turner syndrome. Despite the ANA positivity and thyroid auto-antibody positivity found in patients diagnosed with lichen sclerosis, there is not adequate data suggesting that the disease in the vulva is of autoimmune origin. Recent studies focus on epigenetic changes and phenotypic effects.
2. Infection
Several infectious agents have been considered to be associated with lichen sclerosis. These include pleiomorphic and variable acid-fast bacilli and spirochetes. Studies have revealed a relationship between lichen sclerosus and Borrelia burgdorferi infection, which causes “Acrodermatitis chronica atrophicans” disease. However, serology and polymerase chain reaction (PCR) tests have not confirmed this in a way that leaves no doubt.
Viral agents have been studied, as well. Suspicions about Human Papilloma Virus (HPV) are the strongest ones. Children with lichen sclerosis have been found to more likely to carry HPV compared to other healthy populations. Lichen disease has also been found to develop in the traces of herpes zoster, but it has not been proven that it was due to the permanence of varicella zoster. In addition, a possible relationship between Hepatitis C (HCV) and lichen has been investigated. The link between HCV hepatitis and autoimmunity is also well known. Lichen disease may be associated with autoimmune reactions developed by HCV.
3. Hormonal Effects
The highest incidence rate of lichen sclerosus in women is observed during the periods when estrogen levels are low. The fact that it is seen frequently in pre-adolescence and menopausal period indicates the existence of a relationship between LS and hormonal levels. However, LS has no relationship with pregnancy, hysterectomy (removal of the uterine),hormonal contraceptive (pregnancy prevention) methods. However, it is known that topical applications (like applying creams) intended for providing hormonal support have a positive effect on healing.
4. Regional Factors
The “Koebner phenomenon” was initially described in the development of psoriasis lesions. It is defined as the appearance of new skin lesions, i.e. the disease, on previously unaffected skin following a trauma. As in the Koebner phenomenon, post-traumatic lesions are observed to be exacerbated. Cases where lichen sclerosus disease develops following sunburn, radiation exposure and vulvectomy support this hypothesis.
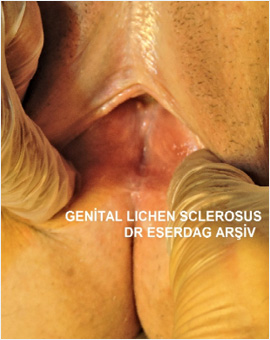
The well-defined external appearance of vulvar lichen sclerosus is white sclerotic plaques which develop on an atrophic, wrinkled background.
However, there are some other appearances including;
A definitive diagnosis can be made through a skin biopsy in any suspected case.
In addition to clinical findings, some clues are also important for the diagnosis of genital lichen sclerosus disease. These include the Koebner phenomenon and the Dermoscopy technique.
It is a condition seen in patients with dermatologic diseases, which is defined as the appearance of the symptoms of the disease after a trauma. Koebner phenomenon is positive in vulvar lichen sclerosus. This is why the disease develops in the perianal area (around the anus),which is the area most exposed to pressure or trauma.
It is the microscopic examination of the superficial skin. The findings obtained through dermoscopic examination of the genital area include “comedone”-like openings, purpura globules, ice slivers, and sparse fine veins on irregular white backgrounds.
The definitive diagnosis of lichen sclerosus is made by skin biopsy. The biopsy sample taken from the densest white area during the examination is sent to a laboratory for pathological examination. During the examinations under the microscope, certain findings are observed such as;
After the treatment changes and improvements are observed in these pathological findings. Therefore, the first biopsy is of great importance in patients who have never been treated. In addition, regular biopsy is important in terms of response of patients to treatment and their follow-up.
In children, a general examination is usually adequate for diagnosis. Biopsy is not preferred because it would lead to a traumatic process. No canceration has been observed in the genital area in childhood. Eczema and vitiligo should also be kept in mind in terms of differential diagnosis.
Among all cases in the childhood age group, the incidence of vulvar lichen sclerosus is between 7 and 15%. Lichen sclerosus is also known to rarely involve areas other than the genital area in childhood.
In childhood, extra-genital involvement is 6%. Until recently, the childhood genital lichen had been thought to disappear with the beginning of the adolescence period. However, according to the current data, lichen sclerosus in childhood can also cause vaginal stenosis at advanced ages.
Itching and pain are the most common symptoms of VLS in children. Other findings are purpura, bleeding, dysuria, constipation, genital erosions and extra-genital complaints. Therefore, lots of people apply to urology and gastroenterology departments frequently. According to studies, its diagnosis is made at 5 years of age an average. Generally, the complaints of the patients cannot be clearly understood and diagnosed until this period.
Lesions and bleeding in genital area of children can be confused with child abuse. Purpura and fissure formation appear to be more severe than normal skin and heal later. In case of such a suspicion, a definitive diagnosis is obtained by biopsy.
Histopathological findings and morphological appearance in the childhood group are the same as in adults. It usually involves the vulva, perineum and perianal region. The clitoris is buried, the labia minora are indistinct, and fissures develop in the perineum. Difficulty in urination and constipation are more common in children.
The course of pediatric vulvar sclerosus is the same as in adults. When untreated, it tends to progress and cause permanent damage. Malignant transformation (canceration) has not been reported. However, scientific studies have shown that children diagnosed with this disease are at a higher risk of encountering HPV types with high oncogenic potential in advanced ages.
Claims that vulvar lichen sclerosis improves with puberty are no longer accepted. However, it is an accepted opinion today that the symptoms ease or the disease goes into recovery process during puberty. Unlike the adult type, childhood vulvar sclerosis does not become cancerous and does not require biopsy follow-up.
There are many dermatological diseases to exclude in the differential diagnosis in adults. It may give common findings with all skin diseases, which involve 'lichenification' findings. Most often it can be confused with dermatitis in atopic individuals. In addition, its differential diagnosis should be made for extra-breast Paget's disease, vitiligo, psoriasis, non-pigmented seborrheic keratosis, genital warts and vulvar intraepithelial neoplasia. It can be difficult to distinguish it from lichen planus. Graft versus host disease, mucosal pemphigoid and lichen planus are diseases that leave more severe scars than vulvar lichen. Nevertheless, they should be considered in differential diagnosis, as well.
Lichen-like symptoms can be observed due to estrogen hormone deficiency during perimenopausal and post-menopausal periods. The indistinctness in the labia minora, vaginal introital stenosis, and dryness and cracks in the skin are the changes that can develop due to hormone deficiency. Patients can be diagnosed late during this period.
The following procedures are available in our Istanbul and Ankara clinics for the treatment of Lichen sclerosus;
Sometimes, we can get better results by combining several of these treatment procedures. In addition, treatments with topical creams and dietary support suitable for lichen are provided. Lichen sclerosus treatment is discussed in a separate article on our website.